Your Quick Guide
- Understanding the Landscape: Cancers That Primarily Affect Women
- Beyond Biology: The Female-Centric Risk Factors
- The Symptoms You Should Never, Ever Ignore
- Diagnosis: What Actually Happens?
- The Treatment Maze: More Than Just Medicine
- The Invisible Battle: Emotional and Mental Health
- Life After Active Treatment: The "New Normal"
- Building Your Support System: It's Not a Solo Mission
- Answers to Questions Women Actually Ask
- Wrapping This Up (Without a Pretty Bow)
Let's talk about something real. Cancer. When it's about women, the conversation feels different, doesn't it? It's not just a medical chart; it's about moms, daughters, sisters, friends. The fear feels sharper, maybe because we're often the caregivers, the ones holding everything together. The phrase "cancer female" gets tossed around in doctor's offices and support groups, but what does it truly encompass? It's more than a diagnosis; it's a life-altering experience that touches every corner of a woman's world—her body, her mind, her family, her future.
I've spent years talking to women on this path, and if there's one thing I've learned, it's that information is the first weapon against the fear. Not just any information, but the kind that speaks to the unique reality of being a woman with cancer. The worries about fertility during treatment, the changes in how you see yourself in the mirror, the sheer exhaustion of managing a household while fighting for your life. This guide is for anyone who's looking for that—a comprehensive, no-nonsense look at what it means to face cancer as a woman. We're going to move past the dry statistics and into the stuff that actually matters when you're sitting in a waiting room or lying awake at 3 AM.
Here’s the thing they don't always tell you upfront: The journey of a cancer female patient is layered. It's biology, for sure—specific organs, specific risks. But it's also psychology, sociology, and plain old logistics. We'll get into all of it.
Understanding the Landscape: Cancers That Primarily Affect Women
Okay, first things first. When we talk about female cancers, we're usually referring to cancers of the reproductive system and breasts. But it's crucial to remember that women get all types of cancer. The experience, however, is often filtered through this female lens. Let's break down the big ones.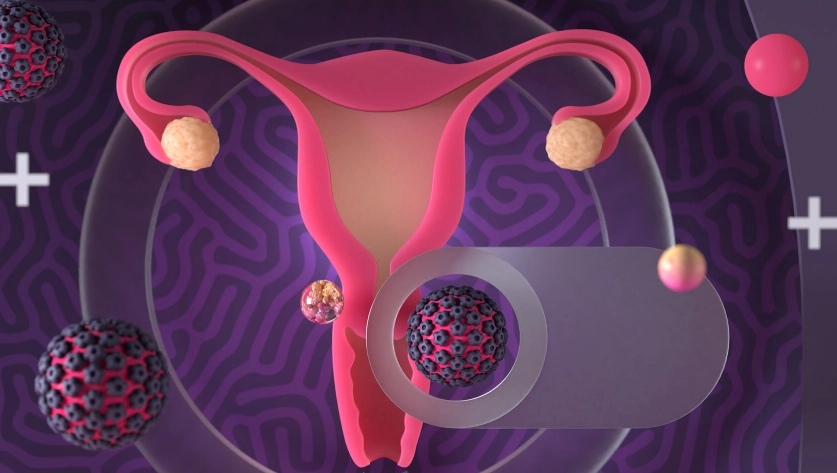
Breast Cancer: The One Everyone Knows About (But Do We Really?)
It's the most common cancer among women worldwide. You know the pink ribbons. But behind the awareness campaigns, there's a complex reality. Not all breast cancers are the same. Some are fueled by hormones (ER/PR-positive), some have a protein called HER2, and some, called triple-negative, are more aggressive and harder to treat. The treatment for a young woman hoping to have children will look wildly different from that for a post-menopausal woman. That's the first layer of personalization for a cancer female facing this diagnosis.
And the stats? While they can be scary, they're also improving. According to the American Cancer Society, the 5-year relative survival rate for localized breast cancer is now 99%. That's huge. But "localized" is the key word there—which is why knowing your body and screening are non-negotiable.
Gynecologic Cancers: Ovarian, Cervical, Uterine
This is where things get tricky because symptoms can be sneaky, often written off as "just period problems" or stress.
Ovarian cancer is called the "silent killer" for a reason, though many women report subtle, persistent signs like bloating, pelvic pain, feeling full quickly, and urinary urgency. The problem is, by the time it's obvious, it's often advanced. There's no reliable screening test for the average woman, which is frankly frustrating and scary.
Cervical cancer is a different story. We have a powerful prevention tool: the HPV vaccine. And screening via Pap smears and HPV tests is highly effective at catching pre-cancerous changes. This is a cancer we can actually beat before it starts, which is a massive public health victory.
Endometrial (Uterine) cancer is the most common gynecologic cancer in the U.S. A major red flag is abnormal vaginal bleeding, especially after menopause. Obesity is a significant risk factor here, which adds another layer of complexity and, sometimes, unwarranted stigma for the cancer female patient.
Quick Reality Check: While these are termed "female cancers," it's vital to acknowledge transgender men and non-binary individuals assigned female at birth who may also face these risks and need culturally competent, sensitive care. The medical system is still catching up on this front.
Beyond Biology: The Female-Centric Risk Factors
We can't just talk about body parts. We have to talk about life stages and hormones, because for women, they're powerful drivers of cancer risk.
Your reproductive history matters. Early menstruation (before 12) and late menopause (after 55) mean more lifetime exposure to estrogen, which can increase breast and endometrial cancer risk. Never having carried a pregnancy to term or having your first child after 30 also modestly increases breast cancer risk. It feels unfair, right? Like your body's natural rhythms are working against you.
Then there's hormone replacement therapy (HRT) for menopause symptoms. The landmark Women's Health Initiative study in the early 2000s really shook things up, linking combined estrogen-plus-progestin therapy to a higher risk of breast cancer. It threw millions of women and their doctors into a dilemma: treat the crushing hot flashes and protect bone health, or avoid a potential cancer risk? The decision is intensely personal and must be made with a good doctor, weighing your individual and family history.
See what I mean? It's never just one thing.
The Symptoms You Should Never, Ever Ignore
I'm not here to make you a hypochondriac. But I am here to tell you to trust your gut. Women are often socialized to downplay their pain, to put others first. When it comes to cancer, that instinct can be deadly. Here’s a shortlist of signs that warrant a doctor's visit, pronto.
- A new lump or thickening in or near your breast or under your arm. And don't just check the breasts—check the area around them, up to the collarbone.
- Any change in the size, shape, or look of your breast or nipple. Dimpling, puckering, redness, or scaling of the skin.
- Unexplained vaginal bleeding or discharge. Spotting between periods, heavy periods, or any bleeding after menopause is a major red flag.
- Persistent bloating, pelvic or abdominal pain, or feeling full too quickly. If it lasts more than two weeks and isn't your normal, get it checked.
- Ongoing changes in bathroom habits: Constipation, diarrhea, or blood in your stool that won't go away. Yes, colorectal cancer affects women too.
- Constant, nagging fatigue that sleep doesn't fix. The kind of tired that feels bone-deep and different from your usual stress.
Look, I knew a woman who had bloating for months. She thought it was gluten, then stress, then just "getting older." It was stage III ovarian cancer. Her biggest regret wasn't the cancer itself—it was not listening to her body sooner. Don't let that be you.
Diagnosis: What Actually Happens?
So you or someone you love has a suspicious symptom. What's the play-by-play? It usually starts with a conversation and a physical exam. Then comes imaging. For breast concerns, that's a mammogram, maybe an ultrasound or MRI. For gynecologic issues, a transvaginal ultrasound is common.
The word that changes everything: biopsy. A small sample of tissue is taken and sent to a pathologist. Waiting for those results is its own special kind of hell. Days feel like years. When the call comes, make sure you have someone with you, or at least on standby. The information can be a blur.
If it's cancer, you'll get a pathology report. This is your roadmap. It will tell you the type, the grade (how abnormal the cells look), the stage (how far it's spread), and key biomarkers like hormone receptors and HER2 status. Get a copy of this report. Read it. Ask questions about every single line. This isn't a time to be polite or feel like you're bothering the doctor. This is your life.
A crucial piece of advice: Before starting any major treatment, consider getting a second opinion. A good oncologist won't be offended. It's standard practice for a major life decision like this. It can confirm your diagnosis, introduce you to new treatment options, or simply give you peace of mind. For a cancer female patient, this step can be empowering in a situation where you feel you've lost all control.
The Treatment Maze: More Than Just Medicine
Treatment plans are as unique as the women receiving them. They're based on that pathology report, your overall health, and your personal goals. Let's look at the tools in the toolbox.
| Treatment Type | What It Is/Does | Key Considerations for Women |
|---|---|---|
| Surgery | Physical removal of the tumor and sometimes surrounding tissue/lymph nodes. | Lumpectomy vs. Mastectomy: A deeply personal choice involving body image, risk reduction, and recovery. Lymph node removal can cause lymphedema (chronic arm swelling). Fertility preservation (egg/embryo freezing) must be discussed BEFORE surgery/chemo if future pregnancy is desired. |
| Chemotherapy | Powerful drugs that kill fast-dividing cells throughout the body. | Often causes immediate menopause and infertility in pre-menopausal women. Hair loss is a profound emotional blow for many. Can cause "chemo brain"—memory and concentration fog. |
| Radiation Therapy | High-energy rays target and destroy cancer cells in a specific area. | For breast cancer, can cause skin changes (like a sunburn), fatigue, and long-term firmness or discoloration of the breast tissue. For pelvic radiation, can lead to vaginal dryness, stenosis (narrowing), and impact bladder/bowel function. |
| Hormone Therapy | Blocks hormones (estrogen/progesterone) from fueling cancer growth. | Used for ER/PR-positive cancers. Drugs like Tamoxifen or Aromatase Inhibitors (Anastrozole, Letrozole) can cause menopausal symptoms (hot flashes, night sweats), joint pain, and bone thinning. Taken for 5-10 years. |
| Targeted Therapy & Immunotherapy | Newer drugs targeting specific cancer cell mutations or boosting the immune system. | More precise, often with different side effects than chemo (e.g., skin rashes, high blood pressure, fatigue). Availability depends on the specific biomarkers of your tumor. |
The side effects column isn't there to scare you. It's there to prepare you. Forewarned is forearmed. For instance, knowing that joint pain is a common side effect of aromatase inhibitors can keep you from thinking the cancer has spread to your bones. It's just the medication, and there are ways to manage it.
The Conversation About Fertility
This one hits hard. If you're a young woman diagnosed with cancer, the question of children can feel as heavy as the disease itself. Oncologists are getting better at this, but you often have to bring it up. Ask, "How will this treatment affect my ability to have children later?" before you start. Options like egg or embryo freezing exist, but they take time (2-4 weeks) and money. Some insurance covers it, some doesn't. It's an added layer of stress on an already impossible situation, but for many, it's a lifeline to a future they still hope to have.
The Invisible Battle: Emotional and Mental Health
Let's be blunt: the mental load of cancer can be as debilitating as the physical effects. We're talking about anxiety that clenches your stomach, depression that makes the world gray, and fear of recurrence that shadows every ache and pain for years afterward.
Body image takes a massive hit. Scars, hair loss, weight changes, the loss of breasts or ovaries—these aren't just physical changes; they're assaults on your identity. I've talked to women who couldn't look at themselves in the mirror for months. Who felt like a stranger in their own body. This is a core part of the cancer female experience that often gets minimized in the rush to treat the disease.
Then there's the relationship strain. Partners don't know what to say or do. You might not want to be touched. Intimacy can feel like a distant memory, especially with vaginal dryness or pain from treatments. Friends might fade away, unsure how to act. Or worse, they offer toxic positivity—"Just stay positive!"—which can make you feel guilty for having perfectly normal sad or angry days.
What helps? Honestly, therapy. Specifically, a therapist who specializes in chronic illness or oncology. Support groups, either in-person or online, can be lifelines. Finding people who get it, without you having to explain a thing. And sometimes, just giving yourself permission to have a really, really bad day.
Life After Active Treatment: The "New Normal"
The last chemo drip, the final radiation zap—you think you'll feel elated. And sometimes you do. But often, there's a weird letdown. You're sent back into the world, but you're not the same person. Your medical team, which was your safety net, sees you less often. This transition can be terrifying. They call it "survivorship," and it comes with its own set of challenges.
You'll have a follow-up schedule—scans and blood tests every few months, then annually. Every scan brings "scanxiety," the days or weeks of dread waiting for results. It's normal. Managing long-term side effects is a new job: combating fatigue, dealing with neuropathy (tingling in hands/feet), managing menopausal symptoms, strengthening bones weakened by hormone therapy.
Lifestyle becomes medicine. Nutrition isn't just about eating; it's about fueling recovery and reducing inflammation. A diet rich in plants, lean proteins, and healthy fats is the general guidance. The National Cancer Institute has solid, evidence-based resources on diet and cancer. Exercise, even gentle walking, is proven to reduce fatigue and improve mood. It's not about being an athlete; it's about moving your body in a way that feels good.
My two cents on the "positive thinking" pressure: It's overrated. Resilience isn't about being happy all the time. It's about getting through the day when you feel like crap. It's about crying in the shower and then making dinner anyway. Give yourself a break from the pressure to be inspiring. Just be you, however messy that is.
Building Your Support System: It's Not a Solo Mission
No woman should go through this alone. But building a team is work. Your medical team is one part. Your personal team is another.
- The Practical Helper: The friend who sets up a meal train, drives you to appointments, or picks up your kids. Let them help. People want to, they just don't know how.
- The Emotional Anchor: The person you can call at 2 AM to say you're scared. Who listens without trying to fix it.
- The Information Partner: Maybe your spouse or a detail-oriented friend who can come to appointments, take notes, and help you research options.
- Professional Support: An oncology social worker. They are unsung heroes who can help with everything from counseling to navigating insurance and finding financial aid.
Online communities can be amazing (like BreastCancer.org or specific forums), but beware of doom-scrolling. It's easy to fall into rabbit holes of worst-case scenarios. Set boundaries for your online time.
Answers to Questions Women Actually Ask
Wrapping This Up (Without a Pretty Bow)
There's no sugar-coating it. A cancer diagnosis as a woman is a seismic event. It reshapes your landscape. But within that truth, there is also room for grit, for connection, for moments of unexpected grace, and for a strength you never knew you had.
The path of a cancer female is uniquely challenging, woven with biological, emotional, and social threads. From understanding the specific risks in your body to advocating for your needs in the treatment room, from weathering the storm of side effects to piecing together a life on the other side—it's a marathon, not a sprint.
Use this information not as a source of fear, but as a map. Ask the hard questions. Build your village. Honor your feelings, all of them. And remember, you are more than your diagnosis. You are a woman navigating one of life's toughest journeys, and that, in itself, is a story of profound courage.
Take it one day, sometimes one hour, at a time. You've got this.